Lea este artículo en español.
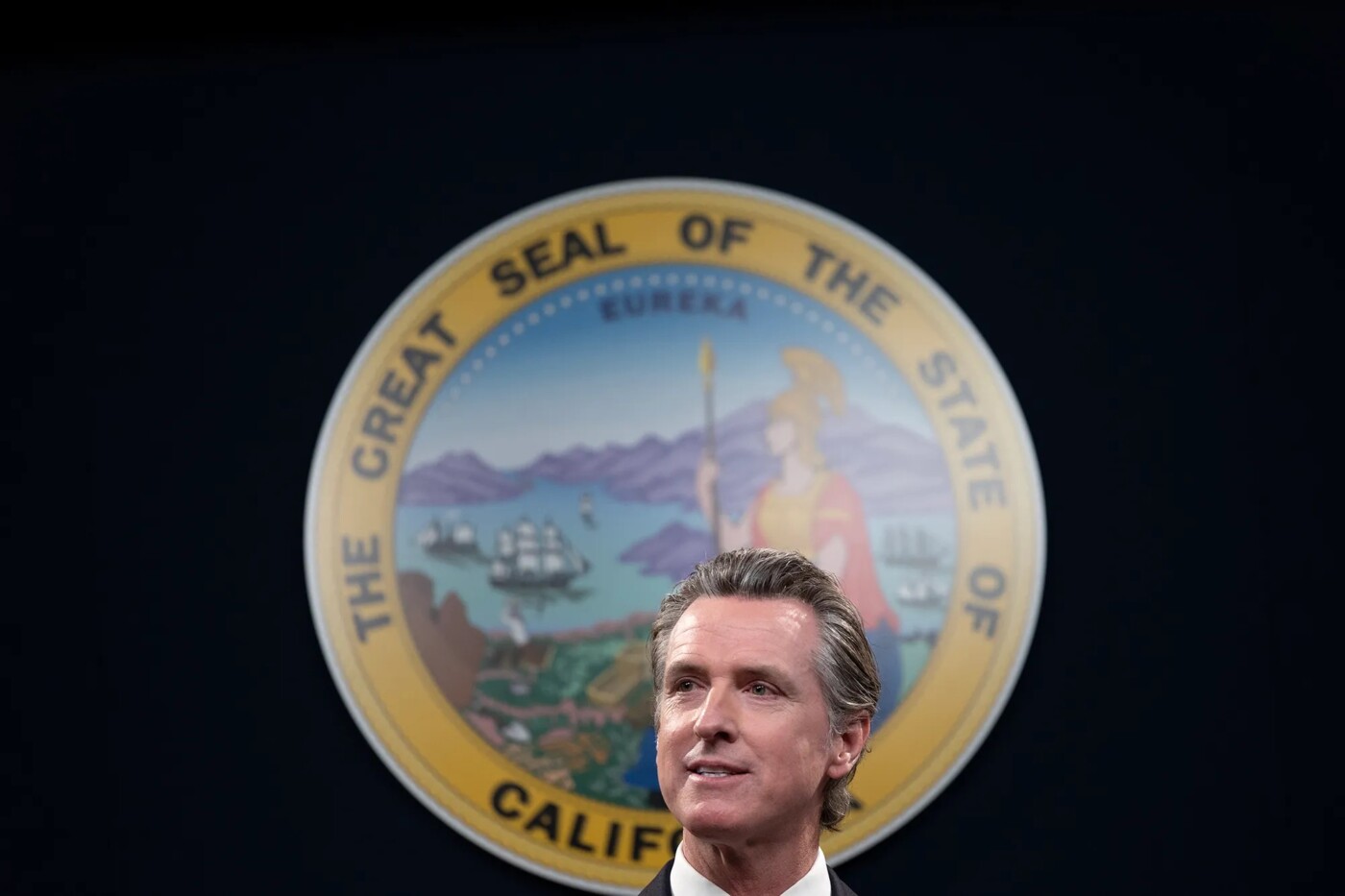
For the second time in as many years, Gov. Gavin Newsom is pushing for major reform of California’s mental health system, this time by overhauling the way counties spend mental health dollars and placing a bond measure before voters to build more psychiatric beds.
County behavioral health advocates and local service providers fear programs will be cut, and, much like the controversial CARE Courts legislation — which passed last year and allows individuals to petition a court to force seriously mentally ill people into treatment and housing — say Newsom’s initial announcement came as a shock.
“We listened to the press conference just like you,” said Christine Stoner-Mertz, executive director of the California Alliance of Child and Family Services, which represents organizations that provide child welfare, foster care, juvenile justice and youth behavioral health services.
The proposal is being pitched as a solution to the state’s ballooning homelessness crisis, but experts doubt it will make any kind of meaningful dent. No one has published bill language for the proposal, but Newsom unveiled two major changes during his March state-of-the-state tour:
- Divert 30% of existing Mental Health Services Act money toward housing people living on the streets who are severely mentally ill;
- Use a bond measure to generate between $3 billion and $5 billion for 6,000 residential psychiatric treatment beds.
Voters passed the Mental Health Services Act nearly two decades ago as a ballot initiative that levied a 1% tax on state millionaires to fund local mental health programs. Substantial changes to the act are subject to voter approval because it originally passed as a ballot measure in 2004.
The proposal aims to reprioritize a significant portion of the state’s existing behavioral health system to focus on what Newsom characterized as the state’s “most acute challenge,” which is the number of homeless people with mental illness and substance use disorders. Only about 20% of California’s approximately 172,000 homeless people have a severe mental illness, according to the U.S. Department of Housing and Urban Development, but the issue plays an outsized role in state politics.
“It’s unacceptable what we’re dealing with at scale now in the state of California,” Newsom said. “We have to address and come to grips with the reality of mental health in this state and our nation.”
Newsom, who made reducing homelessness a key part of his gubernatorial campaign in 2018, is contending with the reality of homelessness increasing by nearly 32% in the past four years. Though he has called out counties for not acting aggressively enough and dedicated nearly $10 billion to address the problem, he has also faced harsh bi-partisan criticism for what many view as a political stunt in threatening to withhold money from counties and failing to significantly increase the state’s housing stock.
Newsom’s proposal is backed by several lawmakers, including former Assemblymember and current Sacramento Mayor Darrell Steinberg, who co-authored the original act, and Sen. Susan Talamantes Eggman, a Democrat from Stockton who co-authored the CARE Court legislation and who has staked the remainder of her term on advancing mental health changes.
Those who do the on-the-ground mental health work in the state, however, say they have major concerns about such a large system shake-up. The focus on housing and the need for more behavioral health treatment beds is welcome, Stoner-Mertz said, but shouldn’t detract from the current workforce crisis and other problems exacerbated by the COVID-19 pandemic.
“One-third is a big chunk of money,” Stoner-Mertz said. “The question in our minds is what is the approach and process to solving some of these problems. We would welcome greater partnership around that.”
What the mental health funding proposal would change
On Wednesday, state officials revealed new details about the proposal. It changes the categories counties would be required to invest in, focusing most of the money on homeless adults. Counties would be required to spend 30%, or roughly $1 billion annually, of their Mental Health Services Act dollars on housing homeless people with serious mental illness or drug addiction. They would also direct 35% of the funds to full-service partnerships for these individuals, which include clinical treatment and social supports co-designed by the client and the program.
The remaining 35% could be used for a combination of existing programs like mental health prevention and early intervention, infrastructure and workforce investments, although officials made it clear that workforce would be a priority. Innovation grants that have historically been part of the program do not have any dedicated funds. The proposal also opens the door to using the money for people who struggle with addiction but don’t have additional mental health needs.
In contrast, current regulations give counties broad flexibility in using the money. A minimum of 38% must be spent on full-service partnerships, although counties can spend up to 70% on these services. (Full-service partnerships are intensive wraparound services designed to do “whatever it takes” to meet the client’s long-term needs. They can include things like 24/7 case management, clinical treatment, and housing.) About 19% is reserved for prevention and early intervention programs, much of which focuses on children, and 5% for innovation. Some counties choose to use a portion of the funds for workforce and infrastructure needs.

There are some concerns about whether counties have historically met minimum spending requirements, particularly for full-service partnerships, but there’s no question that the money has become an integral part of the state’s behavioral health system, making up nearly one-third of all spending. Last year the tax generated about $3.8 billion. Newsom’s proposal introduces standardized accountability measures and reduces the amount of money counties are allowed to keep in reserves.
In addition, language will be placed on the 2024 ballot asking for a general obligation bond to pay for 6,000 psychiatric and substance abuse treatment beds. These beds would serve approximately 10,000 people annually, according to a fact sheet from Newsom’s office, by providing long-term residential treatment. An undetermined portion of the bond funds would be used to house homeless veterans.
For many mental health organizations, the bond to increase residential care capacity is much easier to swallow than prescriptive changes to how mental health dollars are spent. The state faces a shortage of more than 7,700 adult psychiatric beds, according to a 2021 RAND report commissioned by the County Behavioral Health Directors Association.
“We really appreciate the administration looking at the report that we did, and the focus on building out infrastructure is wonderful,” said Michelle Doty Cabrera, executive director of the County Behavioral Health Directors Association. “But we continue to need the same kind of focus on workforce and funding for services ongoing.”
At the same time that Newsom is advancing this proposal, his January budget delays $1.1 billion in other behavioral health investments over the next two years, including money intended to increase treatment capacity for adults and kids in crisis, and money for workforce development.
What are the primary concerns?
There’s no telling how exactly existing mental health priorities will get reallocated, but cuts are nearly inevitable given how heavily counties rely on the dollars. The money is “braided into the fabric of all things in our safety net,” Doty Cabrera said.
But some of the most pressing questions come from those who work with children and families. Currently, at least half of the money earmarked for prevention and early intervention must be used for children and young adults.
“This is the only protection from our perspective that is actually going to keep a focus on young people and keep a focus on more upstream services,” said Adrienne Shilton, director of public policy for the nonprofit California Alliance of Child and Family Services.
That money is potentially on the chopping block under the new proposal, as are innovation grants that have catalyzed multi-county programs to improve services for communities of color and LGBTQ folks.
Historically, Medi-Cal — the state’s public health insurance program for extremely low-income residents — has not covered behavioral health prevention programs, which is where the Mental Health Services Act becomes important. The money was intended to allow counties the greatest amount of flexibility in meeting local needs, particularly when other funding streams came with restrictions, said Toby Ewing, executive director of the Mental Health Services Oversight and Accountability Commission.
“It is designed to be a counterpoint to historic restrictions that were in place for Medi-Cal,” Ewing said.

At the same time that the money gives counties the ability to provide services beyond Medi-Cal, they also use qualifying program expenses to draw down matching Medi-Cal federal funds, effectively expanding local mental health programs. Collectively, counties use about half of the money on services that qualify for matching federal dollars, Doty Cabrera said.
With about $1 billion earmarked for housing, which the federal government will not pay for, the mental health system may face between $500 million and $1 billion in lost federal revenue, Shilton said, if Newsom’s proposal is approved.
Dr. Mark Ghaly, state secretary for Health and Human Services, disagrees with the assumption that these changes mean cuts will happen. The administration’s team has heard the same concerns in stakeholder meetings following the announcement and will work with counties “to try to maintain as much as we possibly can with them,” Ghaly said.
“There is no reason why we won’t be able to do a lot on the prevention and early intervention side,” Ghaly said.
He also notes that this proposal can’t be considered alone. It is part of a larger strategy to improve mental health services in the state, which includes sweeping changes to Medi-Cal, a children’s behavioral health initiative and investments in crisis response. One piece of the puzzle seeks permission from the federal government to use Medi-Cal dollars on housing, which would allow counties to still draw down a significant portion of matching funds.
“All of these things come together, build on each other, and I would like to say catalyze one another to promote the transformation,” Ghaly said. “This is, in my mind, government doing well.”
Will this help homelessness? Not really.
The proposal has been couched as a solution to California’s explosive homelessness problem, which consistently tops the list of voter issues.
“We’re fooling ourselves that if we don’t address that fundamental need that we can turn this thing around,” Newsom said during his press conference, backed by more than a half dozen officials who detailed homeless issues from state, county, city and personal perspectives.
But the public perception that California’s homelessness crisis is caused by psychiatric emergencies and drug addiction is a false one. Rather, decades of politicians upholding restrictive zoning laws and obstructive environmental policies have pushed California to the bottom of affordable housing rankings and are the primary drivers of homelessness in the state. Other factors, like changes to the state’s criminal justice system, also contribute. Dr. Margot Kushel, director of the UC San Francisco Benioff Homelessness and Housing Initiative, said no amount of spending on mental health will improve the state’s overall homelessness problem.
Still, she and other medical professionals who work primarily with unhoused people say the most vulnerable people on the streets are those with untreated mental illness, and prioritizing housing is the most important thing the state can do for that population’s physical and mental health. People living without shelter also face dismal health outcomes, and discharging a patient back to the street is a recipe for swift deterioration.
Even local and county behavioral health groups that have raised concerns about the proposal acknowledge the need for more housing for their clients, but they fear an inversion of the current problem — housing without services — will result.
“My concern is robbing Peter to pay Paul,” said Debbie Manners, president and CEO of Sycamores, a Los Angeles behavioral health and child welfare agency. Sycamores serves about 500 children and families daily through its school-based mental health program. Two years ago the state allocated $4.4 billion to a Children and Youth Behavioral Health Initiative, but it’s a one-time investment.
“I’m not sure how that will fill in the gap. I don’t think it will fill the gap,” Manners said.
Unfortunately, limited funding is the reality of this year’s budget cycle, with the Legislative Analyst’s Office projecting a $24 billion deficit.
“You don’t want to pit one need for money against another, and I get that,” Kushel said. “On the other hand, it isn’t really possible to serve this population without their having housing.”