When California recorded the first U.S. case of COVID-19 more than three years ago, the news was met with fear, confusion and public ire. Schools and businesses closed. State and local officials ordered people to stay home and mask up. Hospitals overflowed with sick and dying patients.
Today, on the last day of the state’s emergency order, much of public life has returned to normal. But for many communities around the state, the disappearance of COVID-19 resources is merely a reminder that the health disparities highlighted during the pandemic are long-entrenched.
“People who were in the gap are going to go back into the gap,” said Kim Rhoads, a physician and associate public health professor at UC San Francisco who has worked throughout the pandemic to make tests and vaccines more accessible to Black and brown neighborhoods in the Bay Area. “There’s going to be a noticeable difference in access.”
The end of the emergency order marks a drastic change in the state’s strategy for managing a virus that has exacted a devastating toll: 100,187 deaths.
Moving forward, the state will lean on its $3.2 billion long-term COVID-19 plan, which involves stockpiling masks and vaccines, but public health agencies will no longer serve as the primary provider of COVID-19 care.
Already, the state has closed all but six OptumServe testing and vaccination centers, according to its appointment website. In an unsigned email, state public health officials acknowledged the “very real toll the pandemic has taken on Californians,” but remained confident its long-term strategy would be sufficient.
“California is equipped to manage the spread of COVID-19, and to continue to limit hospitalizations and deaths as much as possible,” the email stated. Health department officials refused an interview request.
Other resources have dried up as well. Community organizations and local public health departments told CalMatters that money for COVID-19 outreach and response has either already run out or will be gone by summer. Federal support will also expire when the nationwide emergency ends in May.
“After the (state of emergency) ends, there’s not going to be any more substantial money given to COVID-19,” said Bernadette Boden-Albala, dean of UC Irvine’s public health program. “All of the attempts to get information out, to vaccinate folks in harder-to-reach communities, is going to get much harder and at best will be forced into other programs.”
‘Gaps’ in COVID-19 care likely
Traditionally, public health departments have never been direct service providers. Mass vaccine clinics and test-to-treat sites were a modern-day anomaly necessitated by the virus’ aggressive infection rate. Absent funding, much of that work will stop.
During a monthly meeting with county health officers, Assistant State Public Health Officer Dr. Rita Nguyen acknowledged there will be “gaps” in services as public health steps back.
“There will be a big transition. I don’t think it will be smooth. I think we’re all doing the best that we can to help with that transition, but (for) a lot of the services we will not be able to support at the level that we have before,” Nguyen said. “That’s where we’re trying to engage our partners and say ‘We won’t be in this space in a few months. What else can you do to keep work going in this space?’”
At the county level, much of the work involving COVID-19 care has already “significantly scaled down,” said Lizelle Lirio de Luna, director of family health services in San Mateo County. Her division oversaw the vaccination program for the county and doled out more than 185,000 shots. San Mateo’s vaccine clinics will end in March, and COVID-19 grants will be used up by June.
“It’s still evolving what our role will be, but our primary role will not be how it has been where we deliver the direct vaccination service,” De Luna said.
Public health will largely return to its typical role of monitoring infectious diseases of all types, investigating outbreaks, communicating the importance of vaccination and supporting medical providers when necessary — similar to the role it plays during flu season. But local officials, while cautious, were quick to assure that some level of service will be available.
“Because there is an end of a public health emergency doesn’t mean our work ends,” said Rosyo Ramirez, deputy director of community health in Imperial County. “We’ll continue to work as we have been in trying to prevent serious illness.”
The last state-funded testing and treatment sites in Imperial County will close in the beginning of March, Ramirez said, and people will need to go to their medical provider for care. Statewide, the majority of sites closed in January. Imperial’s COVID-19 money will run out in July.
The message to the public is clear: Go see a doctor for your COVID-19 needs.
That message, however, is fraught with uncertainty, about who, if anyone, will step up to fill health care gaps that predated the pandemic. Although medical providers have far more built-in infrastructure to conduct tests and give vaccines than they did three years ago, many people struggle with regular access to health care — particularly those living in rural areas of the state, those who are uninsured and those who can’t afford out-of-pocket charges.
“Everything is moving towards commercialization,” Rhoads with UCSF said.
“All of the resources for COVID are getting pushed into your doctor’s office, so you have to have a doctor….We’re shoving a public health function into health care, and public health and health care are two totally different things.”
Disparities largely unchanged
Though the state poured billions of dollars into COVID-19 emergency response and economic relief efforts — much of which focused on equity — many underserved communities are ending the pandemic in the same way they started: with an acute awareness of unmet need.
Early in the pandemic, the virus swept through the ranks of Latino farmworkers, low-wage factory employees, Filipino nurses, undocumented immigrants, Black and Pacific Islander communities, families living in multigenerational housing or cramped quarters, and others unable to work from home or without adequate access to health care. Of the more than 100,000 COVID-19 deaths to date, Pacific Islanders have the highest mortality rate, followed by African Americans and Latinos.
Vaccination rates among these groups continue to trail far behind the state average. Latino residents fall nearly 15 percentage points below the state vaccination rate when it comes to receiving the first two COVID-19 shots. Native American and Black populations fall behind by 13 and 10 points respectively, while white and Asian groups exceed the statewide rate.
When it comes to the booster and bivalent booster doses, the gap widens significantly. Latinos, with the lowest booster rate, fall 10 points below the state average, 18 points behind their white counterparts and 24 points below Asians. White Californians have the highest bivalent booster rate. (Native Hawaiians and Pacific Islanders have been excluded from this analysis due to anomalies in the state data, including more people reporting vaccination than are estimated in the total population.)
Similarly, the state’s vaccine equity metric shows that as subsequent doses of the vaccine were recommended, those in the most disadvantaged group became less and less likely to get additional shots compared to those in the most advantaged group. The equity metric takes into account socioeconomic variables like income and education as well as race.
The growing vaccine disparity is a reflection of decreased access, community organizers and experts say.
“Everyone wants to throw these health problems back to individuals and individual choice. That doesn’t help us serve the population,” UC Irvine Public Health Dean Boden-Albala said. “Disparities are not about the choices you make but about problems in infrastructure.”
In Delano, Loud For Tomorrow, a youth-led civic engagement group, was instrumental in hosting vaccine clinics and disseminating information by knocking on doors and phone banking. But the group’s funding for COVID-19 outreach ended last summer, said Jose Salvador Orellana, co-founder and lead organizer.
“From the beginning we knew state resources were still not at the level that we needed, and our community, specifically Spanish-speaking Latino communities, needed a different approach” including resources to combat disinformation, Orellana said.
While the state health department was an “amazing partner” in supporting Loud For Tomorrow and other groups’ efforts, most of the collaborations have since ended, Orellana said. Funding from private foundations has also dried up.
“The government relies on these nonprofits to connect to the community. They look like the community; they speak the languages our community speaks,” said Diana Otero, senior director of special projects at the Latino Community Foundation. “It’s really sad we don’t have the resources to continue to do this.”
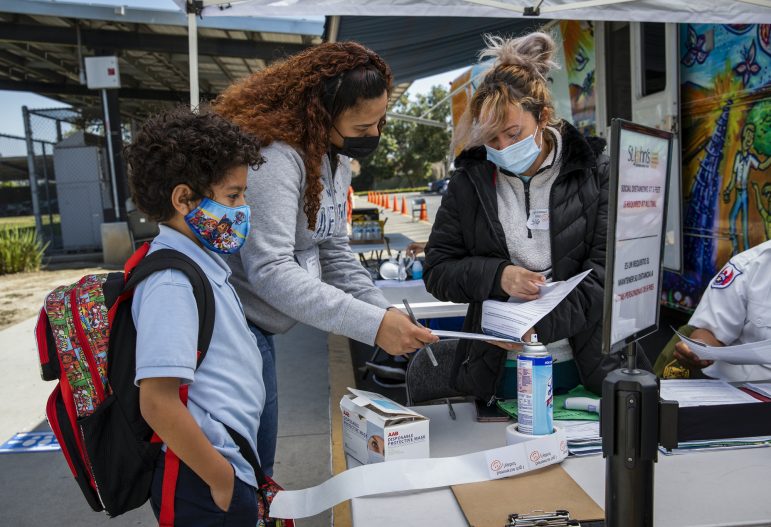
Community groups that received emergency funding now need long-term investments to prevent disparities from worsening, Otero said. In many areas of the state where barriers like cost and distance keep people from accessing traditional brick-and-mortar health care, the COVID-19 clinics run by community organizers have become trusted resource centers.
United Against COVID-19, a coalition of seven community groups in Kern County, held its last vaccine clinic on Feb. 26. The group has vaccinated more than 9,600 people at pop-up clinics in parks and community centers around the county. Throughout the pandemic they’ve vaccinated about 100 people per weekend and continue to see similar numbers of attendees, belying official reports that demand has plummeted. In recent weeks roughly 75% of people coming into the clinics — primarily Latinos — have shown up for booster shots, said Reyna Olaguez, communications manager with Building Healthy Communities Kern, one of the coalition members.
The local health department’s contract with the vaccine provider the coalition uses expired the same day the emergency order ended, but Olaguez said they’re working with the department to use its mobile clinic van in the near future. The schedule won’t be as robust as they’ve been able to maintain — twice a month compared to twice a week — but it’s still important, Olaguez said.
“This work must continue,” Olaguez said. “When it started, it was not ordinary, but now it’s become something that our communities need to get access to health care.”
