
AS THE PANDEMIC drags on, following COVID-19 prevention guidelines can feel like more and more of a challenge.
This kind of fatigue is not unique to pandemic precautions like sticking with social distancing, masking up and keeping your hands washed. With all kinds of health-related behavior changes – including increasing physical activity, eating healthy and decreasing tobacco use – at least half of people relapse within six months.
Think back to the start of April. Much of the United States was under stay-at-home orders. New York City was experiencing close to a thousand COVID-19 deaths a day, and new cases of this previously unknown disease were popping up all over the country.
Coronavirus fears had people either ordering necessities for delivery or rushing through stores as fast as possible, avoiding everyone. When they got home, shoppers wiped down their groceries, vigorously washed hands, maybe even took a shower and changed into clean clothes. People got used to staying home.
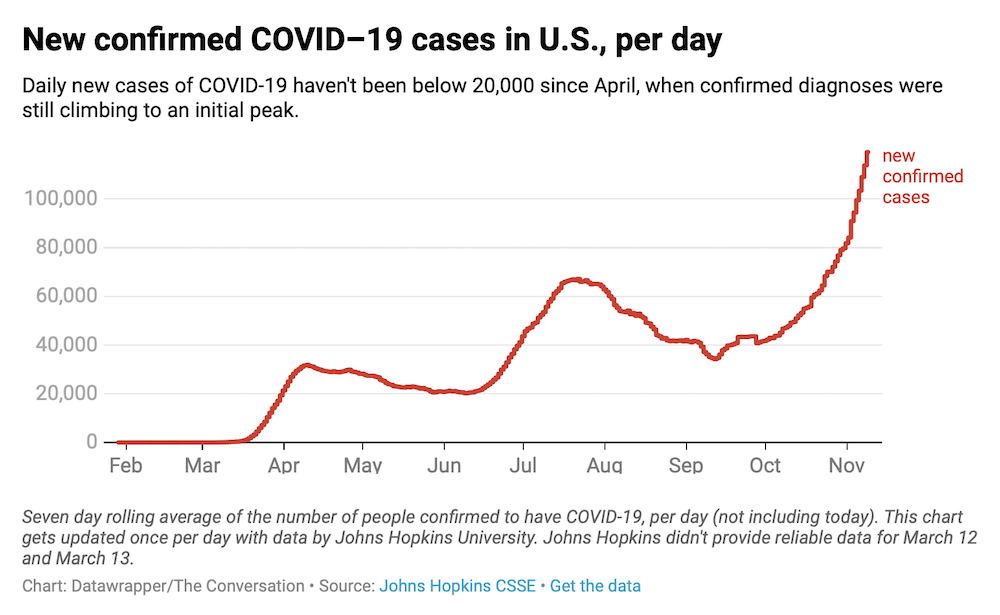
Today, there’s still no cure or vaccine for the coronavirus, and infection numbers are on the rise. Almost a quarter of a million Americans have died from COVID-19 and the risk of infection remains. Now is the time to strengthen your resolve and re-devote yourself to prevention measures.
But fewer in the U.S. are reporting the fear that triggered all those germ-avoiding actions in the spring. Why?
As a public health researcher who investigates health behaviors, I know there are several psychological reasons for why fatigue sets in. Luckily the research also suggests some tactics to help you stay safe as well as protect your mental health and well-being.
How bad is it really?
One explanation for falling off the prevention bandwagon comes down to two important predictors of health behaviors.
- One is perceived susceptibility — how likely do you think you are to get a disease?
- The second is perceived severity — if you do get it, how bad do you think it will it be?
There have been millions of COVID-19 cases in the U.S. But all those people still add up to less than 3% of the country’s total population. Depending where you live, you may know only a few people who have come down with COVID-19, even though the nationwide numbers are high. This can reduce perceived susceptibility.
As doctors learned more about the coronavirus and treatment methods improved, the death rate in the U.S. has also dropped. In May, 6% of diagnosed cases proved fatal, while less than 3% are today. This improvement can reduce perceived severity.
People look at trends like these and let themselves be lulled into believing they’re less susceptible to COVID-19 or that the disease’s severity isn’t that bad. After all, one might reason, it’s been eight months and I haven’t gotten sick.
Everybody else is doing it
Social norms are unwritten rules about how you’re supposed to behave in society. While social norms can be communicated in many ways, one of the main paths is through observational learning. How do others like you behave in similar situations? Seeing that provides you with a road map for your own behavior.
When state governments decide to open bars, restaurants, gyms and movie theaters, you might read it as a signal that these places are now “safe” to visit. Likewise, when you see people socializing without masks and skipping the physical distancing, it looks “normal” and could make you more likely to forgo them yourself. It’s similar to how peer groups strongly affect both alcohol and food consumption.
Yearning to connect
Distancing efforts have increased feelings of social isolation and loneliness for many people, especially among older adults and people who live alone.
Human beings are naturally social animals. So social isolation can be particularly unpleasant. And it can lead to a variety of poor health outcomes including hypertension and poorer sleep. People were able to stop gathering with friends in the spring and avoid get-togethers. But it can be really hard to stick long-term with a behavior that can feel like it’s all downside and no upside.
The trick is to balance physical distancing with social connectedness. Researchers know that reminiscing or having nostalgia about drinking or smoking is one of the major risk factors for relapse.

In the pandemic setting, this is like thinking about the way the world was before COVID-19. A drink after work with a group of friends, a game of pickup basketball or a live concert are all things that people miss in today’s world — and it’s hard not to dwell on the things you’re not getting to do. But while thinking about them can bring back fond memories, it can also encourage you to engage in risky behaviors.
Staying safe and sane
Case counts are rising. The weather is getting colder in many areas, making outdoor dining and socializing less feasible. People need to double down on a level of precaution that can be sustained for months to come, keeping safe while not adding to their social isolation.
Some recommendations must be strictly followed. Hand-washing increased dramatically after the start of the pandemic. Hopefully, this will remain high, since it is a basic way to ward off many infectious diseases and one you can sustain without any negative effects on mental health.
Masks are also important. A study from August showed that 85% of Americans wore masks most of the time in stores. This needs to stay high to help limit the number of new cases.
That leaves physical distancing, which is probably the most difficult. Public health experts often advocate a harm reduction approach for behaviors where abstinence is not feasible — it’s a way to minimize but not eliminate risk. Crowds and large gatherings still need to be avoided. If Zoom and other video chats have grown stale, hosting your own small get-togethers is a possibility. Be aware, though, that while there are ways to minimize the dangers, socializing in a group comes with risks. Remember, your get-together is only as safe as your riskiest friend.
Pandemic fatigue is real, and it’s draining to stay on high alert month after month after month. Understanding it better might help you strengthen your resolve.

Jay Maddock is a professor of public health at Texas A&M University. He does not work for, consult, own shares in or receive funding from any company or organization that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.