Among the most difficult addictions to witness at San Francisco general hospital’s drug clinic is methamphetamine, which leaves users tearing at their skin and unable to eat, sleep, or sign up for help.
The worst part: The clinic workers largely are powerless because unlike with opioid addiction, for which doctors prescribe medications such as methadone, there is no medicine for stimulant use disorder.
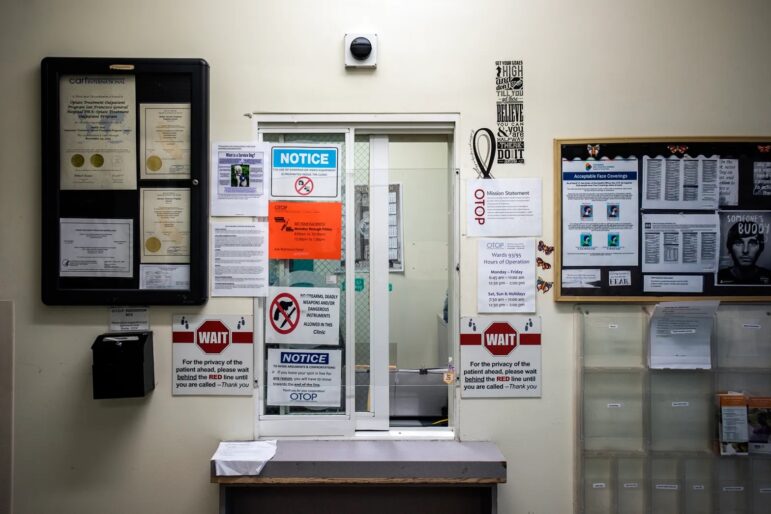
“We live day in and day out watching people suffer in a way that’s hard to imagine,” said Dr. Brad Shapiro, medical director of the Opiate Treatment Outpatient Program at Zuckerberg San Francisco General Hospital. “They’re just dying in front of us.”
Faced with that immense suffering, California will try a new approach to stimulant addiction: Paying people with gift cards to reward them for staying sober.
This model, known as “contingency management,” rewards people with financial incentives each time their drug tests are negative for stimulants. It’s been shown to have success in clinical trials — and the U.S. Department of Veterans Affairs has been using it for more than a decade — but it hasn’t taken off in California. Medicaid previously wouldn’t cover it, so there was no funding to expand its use.
To Shapiro, that’s inexcusable.
“It’s actually, in my opinion, really quite criminal that we’ve gone decades knowing this is an effective treatment and the powers that be have failed to make a pathway for treatment for people,” he said.
The program is expanding now, thanks to a recent waiver by the federal Centers for Medicare & Medicaid Services that allows the agency to cover its costs. California was the first state in the nation to win approval for a contingency management program under Medicaid. The Golden State is launching pilot programs in 24 counties, including San Francisco, Sacramento and Los Angeles. Costs for what collectively is called the Recovery Incentives Program will be reimbursed by CalAIM – the state’s recent expansion of Medi-Cal services.
“All of a sudden we have money to provide this incredibly effective intervention,” said Shapiro, whose clinic is launching one of three pilot programs coming to San Francisco. “So it makes a huge difference.”
Shapiro’s clinic focuses primarily on opioid addiction, but more than half of their patients also have a stimulant use disorder, he said.
While the deadly opioid fentanyl gets most of the attention in the drug epidemic in California and across the country, experts say stimulant use is a major — and growing — concern. In 2021, 65% of drug-related deaths in California involved cocaine, methamphetamine, or other stimulants — up from 22% in 2011, according to the California Department of Health Care Services. Nationally, there were 15,489 overdose deaths involving stimulants other than cocaine (largely methamphetamine) in 2019, up 180% from 2015, according to a study by the National Institute on Drug Abuse.
And with California in the midst of a dire homelessness crisis, stimulants are wreaking havoc on the state’s unhoused community. Among unhoused residents who use drugs, amphetamines are by far the most common choice, according to a recent study by the UCSF Benioff Homelessness and Housing Initiative. Nearly one-third of people surveyed reported using amphetamines three or more times a week, compared to just 11% who used opioids with the same frequency. Some people who live on the street reported using stimulants to stay alert at night, when they fear being attacked if they fall asleep.
To combat stimulant addiction among its patients, Zuckerberg San Francisco General Hospital recently launched a six-month contingency management program as part of the statewide pilot. The hospital opened enrollment on July 17, and staff hope ultimately to serve about 50 people. Clinicians will test participants for stimulants once or twice a week. Each time patients test negative, they’ll get a $10 gift card to Walmart or another retailer. The amount of the gift card gradually will increase, for a maximum of $26.50 per test. If they test positive, they get nothing.
Participants can earn a maximum of $599 over the course of the program. That’s because payments of $600 or more must be reported to the Internal Revenue Service.
Santa Clara County hopes to launch a similar program within the next few weeks. So far this year, 70% of the 120 drug deaths recorded in the county involved methamphetamine, according to the Office of the Medical Examiner-Coroner.
“We’re all excited to try it and see if it does help retain people in treatment for longer periods of time so they are more successful,” said Tammy Ramsey, program manager for the Drug Medi-Cal Organized Delivery System in the county’s behavioral health department.
Other programs in counties throughout California — including Alameda, Fresno, Nevada, Sacramento and Los Angeles — will follow the same model.
If the trials are successful, Shapiro hopes the state will allow them to expand and serve everyone on Medi-Cal.
The model already has proven effective for the Department of Veterans Affairs, according to Dominick DePhilippis, the department’s deputy national mental health director for substance use disorders. The VA started using contingency management in 2011, and as of the beginning of July, the program has treated more than 6,300 veterans. Those veterans have attended about half of their appointments and produced nearly 82,000 urine samples – of which more than 92% were negative for the targeted drug, DePhilippis said.
It’s not just the VA. Of 22 studies testing contingency management’s impact on stimulant addiction, 82% reported “significant increases” in participants’ abstinence, according to a 2021 meta-analysis published in JAMA Psychiatry.

Shapiro believes the model works because it replaces the reward a patient’s brain craves (the drug) with a different type of prize.
“It’s a little bit like winning something,” Shapiro said. “It triggers that reward place in the brain that otherwise they would be turning to the drug for.”
But Tom Wolf, who has battled addiction and homelessness himself and now advocates for drug policy reform, said he worries using Medi-Cal to fund contingency management will create bureaucratic hurdles to treatment as patients wait for the state to decide if they are eligible. Still, he said, the program is worth a shot.
“At this point I’m willing to try it, basically because we have such a dearth of options for people that are struggling with addictions in California,” he said.
Because of how difficult it is to treat his patients that use stimulants — many of them use methamphetamine every day — Shapiro would be happy if even a quarter of participants significantly reduced or stopped using. There is also concern, as with any type of treatment, that patients will relapse once the program is over, he said. To help prevent that, the hospital will provide six additional months of counseling after the contingency management program ends.
Rewarding people for staying sober doesn’t work for everyone. Even before it was covered by Medi-Cal, Zuckerberg San Francisco General Hospital was experimenting with the model in small programs.
One of the participants in those programs, 54-year-old J.W., ended up in the emergency room with heart failure after two decades of methamphetamine use. After his hospital stay, he enrolled in a 12-week program called Heart Plus, which caters to cardiac patients with a history of stimulant use. Every time J.W. did something positive, such as show up to an appointment, take his medication or get a negative drug test, he got to draw a Safeway gift card out of a hat. The cards’ value ranged from $5 to the “elusive” $20, and J.W. — who asked to go by his initials out of fear of being stigmatized for his drug use — estimates he earned about $180 throughout the entire program. He wasn’t working at the time, so the cards helped him get treats such as deli sandwiches and fancy bottles of kombucha.
“It was definitely something to look forward to,” he said. “And it was something fun to spend.”
But it wasn’t enough to get J.W. off drugs. Now that the program has ended, he’s still using methamphetamine — sometimes as often as three times a day — though he says he’s taking smaller doses. And he said he feels much healthier than when he showed up in the emergency room last year, out of breath after the slightest amount of exertion.
J.W. isn’t sure why he didn’t quit using during the program. But methamphetamine has become an entrenched routine in his daily life. He uses upon waking up, in a ritual he compares to having a morning cup of coffee.
“I still kick myself wondering why I didn’t quit altogether,” he said. “There’s no better opportunity.”
