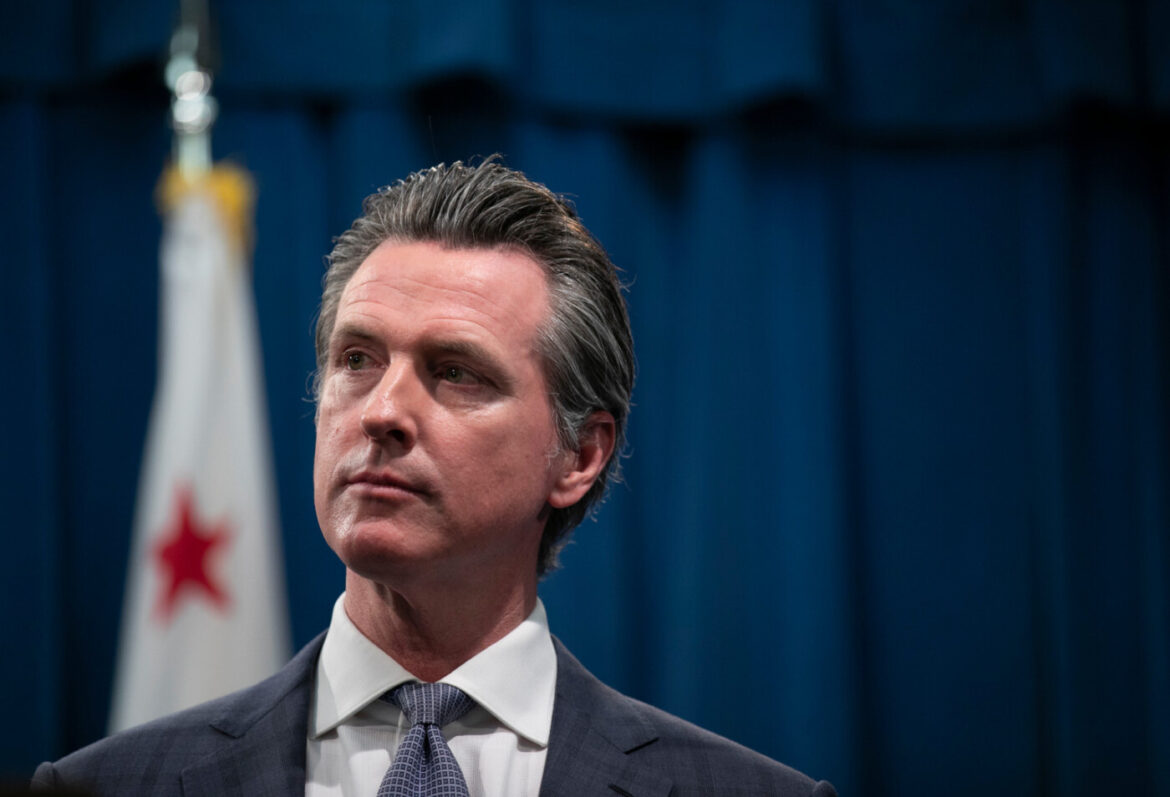
Gov. Gavin Newsom expressed confidence Saturday that California has the capacity to produce enough ventilators to meet its projected needs in response to the coronavirus pandemic. But during a tour of a San Jose energy company that is refurbishing outdated ones, he cautioned that the state’s need could expand significantly if the public doesn’t maintain social distancing and the crisis worsens.
The tour of the Bloom Energy facility demonstrated the state’s ability to leverage its massive technology and manufacturing sector into production or refurbishment of ventilators, something Bloom Energy did this week when it repurposed its fuel-cell manufacturing facility.
“It’s one thing to make new equipment,” Newsom said from a podium positioned in front of stacks of outdated ventilators from the national stockpile. “It’s a challenge to refurbish old equipment.”
Bloom Energy Chief Executive KR Sridhar said his company’s employees had to quickly learn the inner workings of ventilators, a machine they hadn’t worked with before.
“A week ago, none of us knew anything about ventilators other than we knew what it was being used for,” Sridhar said. “But at the end of the day, here’s what we knew. … There are electrical devices, mechanical devices, floor devices. We understand them all.”
Employees had to learn on the job quickly. On Thursday, their first day working in the repurposed facility, Bloom employees refurbished 24 ventilators. On Friday, they refurbished 80, and Sridhar said 120 more would be done by the end of the day Saturday.
“We thought, how difficult can it be, and what’s the worst that can happen,” Sridhar said. “We’re going to try, maybe we fail. But if we’re not training [to refurbish ventilators], we’ve already failed. I don’t care how difficult this problem is. We will solve it.”
Newsom used the language of the tech sector to emphasize that the state must “lean into the future boldly and confidently” and “move at Silicon Valley speed” to “meet the moment” of the coronavirus pandemic. But the bottom line was simple: Newsom believes the state can build and buy its way out of its ventilator shortage.
The state has more than 4,000 ventilators in its stockpile beyond the ones already in hospitals, and Newsom’s goal is to get to 10,000, whether that’s through manufacturing or purchasing ventilators from other countries.
“Thousands more we are confident will be on their way very, very shortly,” Newsom said.
The number of people in intensive care units spiked 105 percent between Friday night and Saturday morning, he said. The state had its 101st death from the virus on Friday night, and Newsom said hospitalizations were up more than 38 percent.
The state had conducted nearly 90,000 tests and had 4,643 confirmed cases as of Friday afternoon.
If Californians practice social distancing, Newsom said the state can cope with the crisis. But “if we’re unsuccessful, the one treatment we know that works? The ventilators. The one treatment we have at our disposal? The ventilators.”

Across the country, the projected need for ventilators has government officials and private industry scrambling to respond. In New York, one hospital has begun sharing ventilators between two patients as the state’s shortage grows.
“Over the course of time, hospitals have understood how many ventilators they actually need,” Dr. Cedric Jamie Rutland, an Irvine-based pulmonary and critical care physician, told CalMatters on Friday. “There’s a rhythm to it, we know who is going to need a vent, but then you introduce a new illness to society and you’ve got these numbers — an exponential increase in the amount of patients who are developing this illness and needing ventilators.”
The danger is when the number of patients needing ventilators exceeds the supply.
“My friends in hospitals in New York have reached that number; out here in California we’re not there yet, but I’m pretty certain we’ll get there,” Rutland said.
And once someone needs a ventilator, they can spend weeks on one, if they get off at all — once patients confirmed to have COVID-19 or displaying its symptoms require a ventilator, the probability of recovery dips significantly.
“What we’re hearing is when you get on a ventilator with COVID-19, that is not a good prognosis. With other diseases it might be a little bit better, but with COVID-19, it seems to be a terrible prognosis overall,” Rutland said.
Another issue is not all physicians and nurses are up to date on how to operate a ventilator. Rutland said he has received messages from colleagues asking for a refresher on how to run one. And appropriate care for someone on a ventilator requires several staff: a respiratory therapist, a nurse and a physician.
“We’re used to having certain [patient-to-staff] ratios,” Rutland said, “but it seems like those ratios are going to get higher as we get more and more patients.”